Influenza kills hundreds of thousands annually and has the potential to cause pandemics, making it a major public health concern. The influenza viruses that infect humans are classified as either A, B or C types based on host tropism and the severity of the disease. Type A can infect a variety of animals as well as humans, and its natural host or reservoir is birds, whereas influenza viruses B and C do not have animal reservoirs. Type A, and to a lesser extent type B, are clinically relevant to humans, with Type C typically causing only mild symptoms.
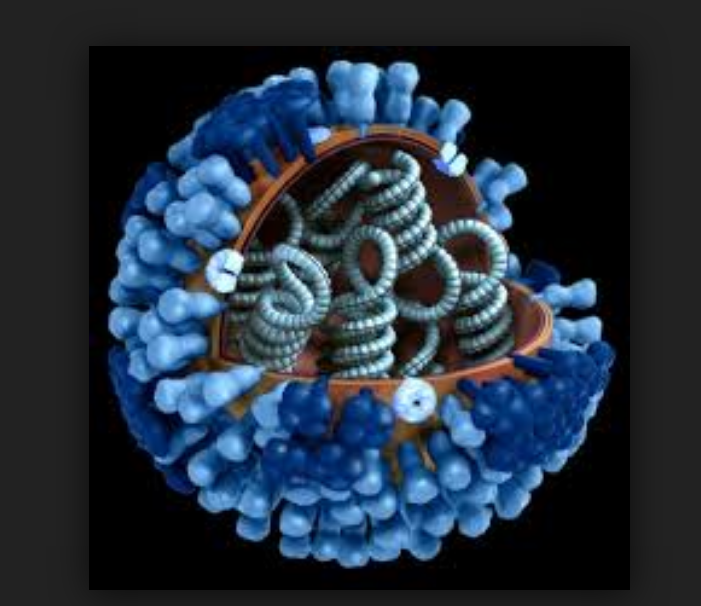
The type A influenza viruses are further divided into subtypes based on the proteins on the virus’ surface: hemagglutinin (HA) and neuraminidase (NA). The HA molecule initiates infection by binding to sialic acid molecules conjugated to many different proteins on the cell surface, thus allowing the virus to enter specific host cells. The NA protein cleaves sialic acid moieties from the cell surface. It prevents the virus from getting trapped into layers of mucus and facilitates virus spread among cells by allowing the release of new progeny from the cell surface to which it may otherwise remain bound through the HA-sialic acid interaction. Infectivity is therefore a fine balance between binding (HA) and letting go (NA) of sialic acid.
Influenza, the challenges
Because of the high mutation rates and re-assortment characteristics of RNA virus genomes, the HA and NA proteins are constantly changing – a phenomenon known as antigenic drift. This drift produces novel strains that can escape the host’s pre-existing immunity. Every flu season, the genetic make-up of the dominant strains from the prior year will have drifted, changing the surface structure of those strains just enough to diminish or even abrogate the effectiveness of the previous year’s vaccine. If the virus can be transmitted easily from person to person, this lack of immunologic experience could result in an epidemic or pandemic.
In addition to producing a large number of mutations, some RNA viruses can exchange genetic material among each other, as well as to acquire genes from their hosts. Rapid change in circulating flu viruses is known as antigenic shift. A shift happens when at least two different strains of influenza combine to form a new virus carrying a mix of the surface antigens of the original strains. This happens quite easily for influenza A as it can infect multiple species and its genome is segmented, meaning that reassortment in a co-infected host can happen more easily. In this case, the human immune system perceives the strain as unfamiliar, and it is this lack of immunologic experience that makes shifted strains so dangerous the moment that they can successfully replicate a spread in a host.
How to combat flu
Currently, there are two main methods of flu prevention and treatment: antivirals and vaccines.
Antivirals
There are two classes of drugs available for the treatment of influenza virus infection: M2 inhibitors and NA inhibitors. These clinically used drugs work by blocking the proton channel activity of the influenza viral M2 protein therefore preventing viral fusion, or by binding to NA to inhibit virus budding. However, for antivirals to be effective against flu, they must be administered within 48 hours of infection. Also, the efficacy of influenza antivirals can be greatly reduced when encountering drug-resistant strains of the virus.
Vaccines
Although not always effective, prevention through seasonal vaccination is the current strategy employed to protect people and contain influenza spread. However, the unstable nature of influenza makes it difficult to control the virus by vaccination. Vaccine manufacturers must reformulate their product every year to account for changes in the virus and to ensure a good match between the HA and NA present in the vaccine and the circulating strain. That is why new vaccine formulations are required in most years. This is a huge task, with vaccination programs against seasonal infections requiring the production of hundreds of million doses within a very short period. In recent years another problem has become apparent: production in eggs, the most common form of large scale manufacturing, can itself cause the loss of critical antigens during the process, making the vaccine less immunogenic than anticipated.
The Holy Grail’ of influenza research
For a long time, scientists have been trying to develop a universal vaccine that would protect people against seasonal flu, and a universal flu vaccine is often referred to as ‘The Holy Grail’ of influenza research. HA protein is often the target of efforts to generate a cross-seasonally protective, universal flu vaccine. This is because the stalk portion of HA (it has a head and stalk, mushroom-like shape) is much more conserved than the variable head portion. Scientists at the National Institutes of Health have developed H1ssF_3928, a candidate universal influenza vaccine that has begun clinical trial to establish its safety and tolerability, as well as its ability to induce an immune response in healthy volunteers, but other candidates are also being investigated. Could flu’s days be numbered?